Vaccination is the introduction of a vaccine into the body to produce immunity to a disease. Vaccine hesitancy is the refusal or delayed acceptance of vaccination due to fears or anxiety about vaccines. It includes a range of concerns such as uncertainty about the contents of vaccines, their safety and the belief that vaccines are responsible for causing other medical conditions (e.g., autism). Other factors include opposition to state control and infringement on individual liberty, suspicions about the pharmaceutical industry and a declining faith in science and medicine. In Canada, as in other wealthy countries, vaccine hesitancy has increased in recent years, including resistance to vaccination among some Canadians during the COVID-19 pandemic.
This is the full-length entry about Vaccination and Vaccine Hesitancy in Canada. For a plain-language summary, please see Vaccination and Vaccine Hesitancy in Canada (Plain-Language Summary).

Vaccine Hesitancy and Herd Immunity
Every year, vaccines prevent an estimated two to three million deaths among young children around the world. Yet experts have noted an increasing trend of vaccine hesitancy in Canada and other wealthy countries. This trend threatens herd immunity and community health.
Herd immunity happens when a large proportion of the community is immune to a disease. This makes it unlikely for the disease to be spread from person to person, protecting those who cannot be vaccinated or who are otherwise vulnerable. In order to achieve herd immunity for measles, for example, approximately 95 per cent of the population must be vaccinated.
Vaccine hesitancy has contributed to a resurgence in measles and other vaccine-preventable diseases in North America and Europe. In 2019, the World Health Organization listed vaccine hesitancy as one of the “Ten Threats to Global Health.”
Vaccine Regulations in Canada
In Canada, vaccination is voluntary. Two provinces — Ontario and New Brunswick — require proof of immunization for children and adolescents to attend school. This includes vaccination for diphtheria, tetanus, polio, measles, mumps and rubella. However, even in these provinces, parents may opt out of vaccinations for medical or ideological reasons.
Vaccine Hesitancy and Outbreaks in Canada
The Canadian government has set a target of 95 per cent coverage for all childhood vaccines. However, according to a 2017 survey by the federal government, vaccine coverage was lower than 95 per cent for all diseases, including measles, mumps, rubella, pertussis, diphtheria and tetanus. According to 2018 estimates from the Organisation for Economic Co-operation and Development (OECD), vaccine coverage in Canada was lower than that of many affluent countries, including New Zealand, Germany, Spain, the Netherlands, the United Kingdom, the United States, Italy, Switzerland, Norway and France.
Since 2005, Canada has suffered from outbreaks of vaccine-preventable diseases. This includes significant measles outbreaks in 2008, 2010–12, 2014, 2015 and 2019. Many of these were linked to communities where vaccination was questioned or discouraged. Similarly, large mumps outbreaks occurred in British Columbia, Alberta, Ontario, Quebec, Nova Scotia and New Brunswick between 2007 and 2010.
Vaccine hesitancy has influenced vaccine uptake in Canada. However, it is important to note that barriers to accessing vaccines and health care also play a role. This is particularly the case in remote communities in Canada.
Reasons for Vaccine Hesitancy
Vaccine hesitancy includes a range of concerns, including uncertainty about vaccines’ contents and their safety. Some people believe that vaccines cause other medical conditions (e.g., autism). Hesitancy can also involve fears about state control and the loss of individual rights. Complacency also plays a role in vaccine hesitancy. So does the rise of “influencer” culture and a declining faith in science and medicine. Parents worry about the possible side effects of vaccinating their children versus the chance of their children contracting a potentially harmful or fatal disease. At the same time, they struggle with their responsibility to the wider community.

Complacency
Vaccines led to the eradication of smallpox in 1980 and the declining incidence of childhood diseases such as polio, diphtheria, and pertussis (whooping cough). However, these very successes have led to complacency. As these diseases no longer appear to be a threat, some people believe that vaccination is unnecessary. Vaccine hesitancy has therefore increased in North America and Europe, where once-common childhood diseases virtually disappeared. This in turn has led to a resurgence of such diseases.
In contrast, vaccine coverage has improved in the Global South, where the World Health Organization, UNICEF, the World Bank, and the Bill & Melinda Gates Foundation partnered with others to form Gavi: The Vaccine Alliance. This alliance has vaccinated over 760 million children. However, the alliance has also been criticized for a “top-down” approach that forces vaccination on individuals and countries. This in turn raises questions about global vaccine initiatives, autonomy, individual rights and the “public good.”
Individual Rights vs. the Public Good
Maintenance of herd immunity is crucial to ensuring the health of people who are immunocompromised or who are allergic to a vaccine. At the heart of the debate about whether individuals have the right to choose not to vaccinate are the concepts of “public good” and “public health.”
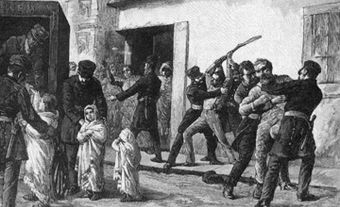
This debate has roots in the 19th century. In the 1800s and 1900s, several countries passed (and enforced) compulsory vaccination laws. These laws were influenced by an emerging belief that health was a public concern, rather than an individual one. Citizens therefore had a responsibility to ensure they were not spreading communicable diseases to their peers. Yet from the beginning, people questioned and protested compulsory vaccination, asserting their individual right to choose. In 19th century Montreal, for example, French Canadians resisted smallpox vaccination. This contributed to high death rates during a smallpox epidemic in 1885. In Britain, resistance led to the amendment of mandatory smallpox vaccination laws to allow conscientious objections in 1898. This was the forerunner of modern vaccine exemptions.
Risk-Benefit
When experts discuss vaccination, they often refer to a risk-benefit relationship. This means the benefit of disease prevention must outweigh the risk of injury or side effects. The medical and scientific consensus is that the risks of vaccination are low. Any vaccine can cause a reaction, but side effects are usually mild. Some examples of a mild side effects include, a low-grade fever or pain at the injection site. In rare cases, vaccines may cause a severe allergic reaction or neurological side effect, like a seizure. However, the risks of naturally contracting diseases like measles or polio are far higher, since the results can be fatal.

Safety Concerns About Early Vaccines
Vaccine hesitancy is not new. In fact, it dates back to the first vaccine for smallpox, which was created in 1796 by Edward Jenner. Unlike today, early vaccines did not have to pass rigorous tests for safety and effectiveness. Therefore, individuals were unsure of their safety and their ability to prevent communicable diseases. (Some individuals also opposed early vaccines on religious grounds due to concerns about the sanctity of the body and maintaining purity.)
In the 20th century, a number of vaccine disasters raised doubts about their safety. This included the Lübeck Disaster in Germany in 1933, where 72 infants died from an improperly manufactured tuberculosis vaccine. During the Cutter Incident in California in 1954, several thousand vaccinated children and community contacts were infected with polio from an improperly manufactured version of Jonas Salk’s polio vaccine. Two hundred people had paralytic symptoms and 10 died. Both cases made the international news, further harming faith in the safety of vaccines.
Vaccines and Autism?
Beginning in the late 1990s, many people became worried about a supposed link between vaccines and autism. This fear stemmed from a 1998 Lancet article written by Andrew Wakefield and co-authors. In this now-debunked article, Wakefield and his co-authors alleged that their research linked vaccination with the measles-mumps-rubella (MMR) vaccine to the onset of symptoms of autism in children. The article did not state that it had evidence of MMR causing autism. However, Wakefield gave several interviews and press statements where he requested the vaccine not be administered until the issue was further investigated. Due to Wakefield’s statements and the uproar about public safety, the article received much attention from scientific researchers and the general public.
In 2010, the article was retracted from the Lancet for ethical violations in patient recruitment. Moreover, subsequent studies showed no connection between autism and the MMR vaccine. Despite this, media coverage of Wakefield’s theory contributed to a widespread belief in such a link.
Influencer Culture and Loss of Faith in Doctors and Science
Though the Wakefield article and its findings have been disproven, it is still influential in anti-vaccine culture. Part of the reason is that several celebrities, including Jim Carrey, have supported Wakefield’s link between the MMR vaccine and autism. The rise of celebrity and “influencer” culture has also highlighted a startling loss of faith in doctors. Some vaccine-hesitant people doubt doctors’ expertise and integrity. They question the links between doctors and “Big Pharma” (pharmaceutical companies) and criticize scientists and medical experts for failing to recognize opposing viewpoints and evidence. Some also accuse doctors and governments of overstepping their bounds in limiting parental rights and independence.
Communication and Trust
While vaccines now have a proven track record as a safe and effective way to prevent communicable diseases, it is a struggle to communicate this to populations in a clear and convincing way. To do so, there must be mutual respect and trust between decision-makers, physicians and the public. Governments and health organizations must also clearly recognize and communicate the complexities and compromise involved in achieving herd immunity, and they must promote a deep understanding of the responsibilities, as well as the rights, of citizenship.
Vaccine Hesitancy and the COVID-19 Pandemic

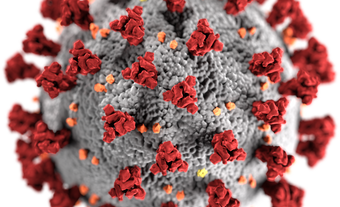
The above factors have affected vaccine uptake and hesitancy during the COVID-19 pandemic (2020–present). In December 2019, a new type of coronavirus, SARS-CoV-2, emerged in China. The virus causes a severe acute respiratory syndrome that was quickly dubbed “coronavirus disease 19” or COVID-19. By March 2023, the virus had caused more than 6.87 million deaths worldwide, including more than 51,447 in Canada.
In December 2020, about a year after the first cases of the virus were reported, the first COVID-19 vaccine was approved for use. By July 2021, approximately 30 such vaccines were approved for use by at least one national regulatory body. Vaccine development continued as the virus mutated, and in September 2022, the first bivalent vaccine (which targets the original virus strain and the Omicron variant) was approved for use in Canada.

Overall, the uptake of COVID-19 vaccines has been high in Canada. As of 3 March 2023, more than 80 per cent of the population had been fully vaccinated (that is, they had either received a single-dose vaccine or both doses of the two-dose vaccines).
Yet a significant proportion of Canadians have either delayed or refused vaccination against COVID-19. This includes people who have otherwise accepted vaccination against influenza and childhood diseases, such as measles and polio. Hesitancy has been influenced by several factors, including mistrust of health care systems and those creating vaccine policy. Widespread vaccination and vaccine mandates have been seen as a violation of individual rights and freedoms. Some suspect the government of using the pandemic to extend its influence and to control individual citizens. This has caused some individuals to believe conspiracy theories and claims that the government is inserting microchips during vaccination to track peoples’ movements.
Another factor is concern about the safety and efficacy of COVID-19 vaccines. While the development and rollout of COVID-19 vaccines was rapid, vaccine development was based on years of mRNA research and a concerted effort by researchers, governments and pharmaceutical companies during the pandemic. Yet some Canadians believe that normal regulations and procedures were circumvented and that COVID-19 vaccines were not rigorously tested. The safety of the mRNA technology used in the Pfizer and Moderna COVID-19 vaccines has also been questioned. Moreover, reports of adverse (though rare) reactions and serious side effects, were widely reported and disseminated via social media.
Safety concerns have affected vaccine uptake among children and youth, who typically develop less serious symptoms from COVID-19. For such groups, the risk-benefit relationship is less clear. Some Canadian parents have therefore decided that vaccine side effects are a greater risk to their children than the virus. By 26 February 2023, only 40.6 per cent of children between the ages of 5 and 11 were fully vaccinated, even though they had been eligible for vaccination for nearly a year (the first vaccine for that age group was approved in November 2021). In contrast, vaccine uptake has been highest among Canadians aged 60 years or older, an age group that is more vulnerable to COVID-19. As of 26 February 2023, more than 90 per cent of this age group were fully vaccinated.
Vaccine uptake has been lower among Black Canadians, Indigenous peoples and newcomers to Canada. Some of these groups have experienced discrimination within public health and the health care system, including a history of medical experimentation and segregation in the postwar years. (See also Racial Segregation of Black People in Canada; Racial Segregation of Indigenous Peoples in Canada.) This has contributed to distrust of government, public health and health care systems, and of vaccines.
Finally, complacency has played a role in vaccine hesitancy. Booster uptake, for example, has been noticeably slower than for the primary series of COVID-19 vaccines. As the pandemic has progressed, vaccination has significantly reduced the risk of serious illness and death among healthy members of the population; moreover, some mutations of the virus seem to cause less severe illness. This has led to a sense of complacency about COVID-19 among many Canadians.

 Share on Facebook
Share on Facebook Share on X
Share on X Share by Email
Share by Email Share on Google Classroom
Share on Google Classroom