In early 2020, as the COVID-19 pandemic accelerated, it seemed very unlikely that a safe and effective vaccine could be developed and deployed within one to two years. A vaccine had never been developed against a new virus during a pandemic, and there was no approved vaccine yet to prevent a coronavirus infection in humans. Despite this, the first COVID-19 vaccine was approved in December 2020, about a year after the first cases were reported. By July 2021, there were more than 30 COVID-19 vaccines authorized for public use by at least one national regulatory authority. This was possible because of decades of research on coronaviruses and vaccine technology — particularly in the use of messenger ribonucleic acid (mRNA) — significant government investment, and unprecedented cooperation between governments and university research labs, pharmaceutical firms and international health organizations. Several Canadian scientists were involved in key elements of the research that led to the mRNA COVID-19 vaccines developed by Pfizer and Moderna.
Click here for definitions of key terms used in this article.

International Cooperation and Government Funding
The SARS-CoV-2 virus genetic sequence was publicly shared on 12 January 2020. This sparked an unprecedented level of government funding and collaboration with university research labs, pharmaceutical firms and international health organizations centred on the research and development of a long list of potential vaccine candidates. By April, there were nearly 80 companies and institutes in 19 countries focused on resolving the COVID-19 vaccine challenge. At this point, the Access to COVID-19 Tools (ACT) Accelerator, an initiative by the World Health Organization and its partners, was launched to facilitate global collaboration to accelerate development, production and equitable access to COVID-19 tests, treatments and vaccines. Then, on 15 May, the U.S. government launched Operation Warp Speed to rapidly develop, produce and distribute safe and effective vaccines, treatments and tests. It helped companies expedite the placement of multiple COVID-19 vaccine candidates into clinical trials by the fall of 2020 and target the manufacture of 300 million doses by January 2021.
Clinical Trials
It typically takes an average of 10 to 15 years to develop a new vaccine, from the initial concept to three phases of clinical trials to regulatory approval, production and distribution to, finally, injection into arms. It is normally a process of clinical trials in linear steps. Phase I primarily tests a vaccine for safety in healthy subjects. Phase II evaluates immune response, dose levels and any adverse effects. Phase III tests the effectiveness of the vaccine to prevent disease transmission and infection. However, to meet the urgency of the pandemic, a process of parallel steps was developed; no step could be shortened or skipped, but they could overlap.
Vaccine Research
There were both new and familiar approaches taken in developing COVID-19 vaccines. One of the most familiar methods was based on inactivating the whole virus to prompt an immune response. Another familiar but newer method used a viral vector (a harmless virus or bacterium) to deliver the genetic material for coding a specific antigen of the infectious virus into the recipient’s host cells to stimulate immunity. However, the most successful approach to a COVID-19 vaccine has been the application of a relatively new process based on the use of messenger RNA (mRNA). Although it may seem new, it was based on decades of research that began in the 1980s and progressed along several separate fronts. One of these research fronts was led by a Canadian group based at the University of British Columbia that, quite literally, provided the key to the success of the mRNA COVID-19 vaccines.
Research and Development of mRNA Technology
Messenger ribonucleic acid (mRNA) is a single-stranded molecule that corresponds to the genetic sequence of a gene that is read by a ribosome (molecular machines that link amino acids together in cells) in the process of synthesizing a specific protein. An mRNA vaccine is designed to deliver molecules of antigen-encoding mRNA into immune cells. These cells then use the specific mRNA as a blueprint to build a distinctive foreign protein that would normally be produced by a pathogen, such as the COVID-19 virus. These proteins stimulate an adaptive immune response that teaches the body’s immune system to recognize and destroy the real pathogen if it enters and infects the body.

The idea of unlocking and synthesizing mRNA to treat diseases and make vaccines emerged in the 1980s. In the 1990s, the research team of biochemist Katalin Karikó and immunologist Drew Weissman at the University of Pennsylvania made important progress in the development of mRNA vaccines. By the mid-1990s, mRNA vaccines had been tested in mice against influenza and cancer. Yet the main challenge limiting the use of mRNA in human vaccines was transporting the mRNA material through the walls of immune cells to safely trigger an effective immune response.
Researchers at the University of British Columbia played an important role in solving the problem of delivering mRNA into immune cells. In 1995, Pieter Cullis and his team, in collaboration with Jeffery Wheeler, focused on the use of lipid nanoparticles (LNPs), which are fatty organic substances utilized by living cells to form a protective bubble around a medicine, particularly gene therapy drugs, so that it could be delivered into cells. By 2005, the UBC group had further developed lipid nanoparticles for a variety of uses. That year, the research team at the University of Pennsylvania made a key breakthrough. They developed a method to produce synthetic mRNA that could safely be injected into cells. (See also Canadian Lipid Nanoparticle Research: The Key to COVID-19 mRNA Vaccines.)
Meanwhile, in 2007, another Canadian, Derrick Rossi, established a laboratory at Harvard Medical School that built on the work of Karikó and Weissman. Rossi’s research utilized mRNA to make adult cells function like embryonic stem cells. This research opened the door to reprogramming cells for many purposes, including repairing damaged tissues and generating human organs for transplantation. From this work, the biotech company Moderna was established in the United States in 2010.
At this point, Cullis’s team joined forces with Karikó and Weissman to focus on mRNA vaccine development that would utilize lipid nanoparticles to encapsulate synthetic mRNA, thus allowing it to safely enter immune cells. This work prompted collaborations with the German biotech company BioNTech and U.S. pharmaceutical firm Pfizer. In 2012, the first successful tests of an mRNA-based vaccine were conducted in mice, followed by the first human trial of the vaccine against influenza in 2015.
Meanwhile, driven by the growing threat of coronaviruses following the SARS outbreak in 2003 and Middle East Respiratory Syndrome (MERS) outbreak in 2012, research began in 2014 at the U.S. National Institutes of Health (NIH) that focused on coronavirus biology and vaccine development. A major outcome of this work involved studies of the signature “spike protein” of the coronavirus and its potential role in vaccine development. This work led to a collaboration between the NIH and Moderna.
Development of COVID-19 Vaccines
The prompt identification of the SARS-CoV-2 virus and public release of its genetic sequence in January 2020 expedited the development of COVID-19 vaccines based on a variety of biotechnologies. Most notably, the rapid spread of the pandemic prompted the interweaving of research threads focused on mRNA-based vaccines and coronavirus biology into accelerated programs at Moderna and Pfizer-BioNTech to develop mRNA COVID-19 vaccines. This work was advanced by initiatives such as Operation Warp Speed. Clinical trials of both mRNA vaccines demonstrated high levels of safety and a remarkable 90 to 95 per cent efficacy in preventing severe infection and death.
On 2 December 2020, about one year after the first COVID-19 cases emerged, the United Kingdom gave emergency-use authorization to the mRNA COVID-19 vaccine produced by Pfizer-BioNTech. Canada followed suit on 9 December, as did the United States on 11 December. The first vaccinations were administered in Canada on December 14 to residents of long-term care homes and front-line health workers. Canadian approval of a second mRNA vaccine, produced by Moderna, was given on 23 December. A third, viral vector-based vaccine, produced by Oxford-AstraZeneca, was approved in Canada on 26 February, while a fourth vaccine, Johnson & Johnson’s single dose vaccine, was approved on 5 March 2021. A protein-based vaccine produced by Novavax Inc was authorized by Health Canada on 17 February 2022. That same month, a plant based vaccine by Medicago Covifenz was approved in Canada.
Globally, as of 4 March 2023, there are 50 COVID-19 vaccines authorized for public use by at least one national regulatory authority, as well as 242 vaccine candidates in various stages of development.
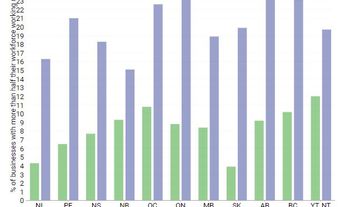
COVID-19 Vaccine Uptake in Canada and Internationally
As of 3 March 2023, 83.4 per cent of Canada’s total population had received at least one dose of a COVID-19 vaccine; of those five years of age and older, it was 87.19 per cent. Of the total population, 80.7 per cent were fully vaccinated (at least two doses); among those five and older, it was 84.5 per cent.
While Canada has achieved one of the highest uptake levels of COVID-19 vaccines internationally, vaccine uptake levels vary widely. As of 8 March 2023, there have been 13.32 billion COVID-19 vaccine doses distributed globally, with 69.7 per cent of the world’s total population having received at least one dose. However, many countries, especially in Africa, have had very low COVID-19 vaccine uptake. A variety of factors have limited and constrained uptake of COVID-19 vaccines in these countries, including difficulties obtaining, storing and distributing vaccines; challenges in delivery and administration of vaccines by public health and medical personnel; and public resistance due to vaccine hesitancy, lack of information or persistent disinformation or misinformation about COVID-19 vaccines. (See also Vaccination and Vaccine Hesitancy in Canada.)
Nevertheless, the development and deployment of safe and effective vaccines against a new and deadly respiratory viral disease like COVID-19, amid an unprecedented pandemic, remains a remarkable and historic achievement.
Key Terms
Pandemic – An outbreak of an infectious disease, usually caused by a new virus or bacterium, or a novel strain, that affects a large proportion of the population in multiple countries or worldwide.
Public Health – Health Services, usually preventative in approach, provided by a government to improve the health of citizens on a population level.
Vaccine – A preparation made from killed or weakened bacteria or virus, or their specific antigens, that stimulates the body to develop immunity to that same bacteria or virus.
Virus – An organism, too small to be seen with a typical microscope, that can multiply inside the cells of its host and usually causes disease.

 Share on Facebook
Share on Facebook Share on X
Share on X Share by Email
Share by Email Share on Google Classroom
Share on Google Classroom