What Is the Flu?
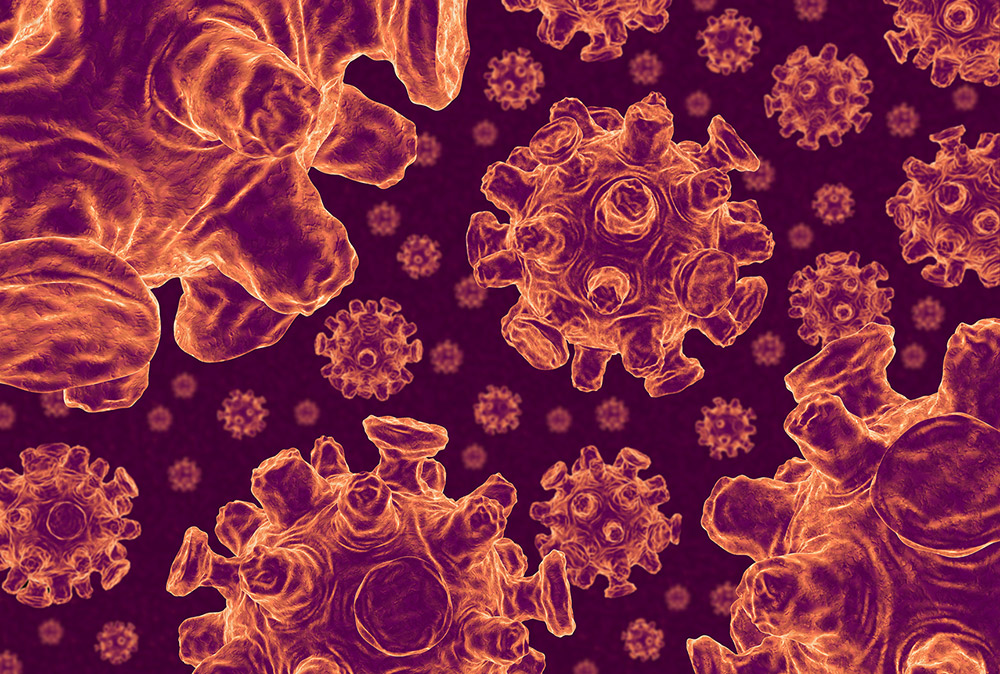
The flu is a contagious respiratory disease. It’s a common illness, caused by viruses belonging to the family Orthomyxoviridae. Within that family there are six genera, or types, four of which cause the flu: influenza A, B, C and D. Influenza A, B and C viruses infect humans, while influenza A can also infect a number of warm-blooded animals, including horses, dogs and birds. In addition, influenza A, C and D can infect pigs, though influenza D, discovered in 2011, is believed to primarily infect cattle. Human influenza pandemics, such as the 1918 Spanish flu, are caused by influenza A.
Nomenclature and Classification
Influenza A viruses are divided into subtypes based on two proteins found on the surface of the virus: hemagglutinin and neuraminidase. There are 18 forms of hemagglutinin and 11 forms of neuraminidase associated with influenza A, numbered H1–18 and N1–11, respectively. Viruses are named for the forms of the proteins they contain. For example, the 1918 pandemic was caused by an H1N1 virus, while H3N8 and H3N2 infect dogs.
Influenza B viruses do not have subtypes but are divided by lineage. There are two lineages of viruses currently circulating, Victoria and Yamagata. Named for where they were first isolated, Victoria viruses originated in Victoria, Australia, while Yamagata viruses were found in Yamagata, Japan.
All types of influenza viruses, A, B, C and D, may include multiple strains. Strains are categorized by listing the type of influenza, the host in which the virus was found (or “isolated”), location of the isolation, an “isolate number” (or lab number), the year, and finally, in the case of influenza A, the subtype. For example, influenza virus A/chicken/Hong Kong/59/1997 (H5N1) was found in chickens in Hong Kong in 1997 and was subtype H5N1, while influenza D/bovine/France/2986/2012 was found in cows in France in 2012. When isolated in humans, the host is left out of the list of designations, such as C/Alberta/10161/2011.
In the case of influenza B, the lineage (Victoria or Yamagata) isn’t listed in a virus’s full name. For example, while B/Brisbane/60/2008 belongs to the Victoria lineage, its name only indicates that it was isolated in Brisbane, Australia, in 2008.
What Are Flu Symptoms?
Flu symptoms include fever, cough, headache, runny nose, body aches and fatigue. Symptoms arrive suddenly and may last for up to a week or more. The disease affects people of all ages but the most vulnerable are the very young, the very old and those with pre-existing illnesses. In climates such as Canada’s, the viruses that circulate each winter are known as the “seasonal flu.” Seasonal flu viruses are primarily caused by influenza A and B (infection by influenza C is less common and causes less severe symptoms).
How Is the Flu Spread?
The flu is spread through contact with infected people or contaminated objects. When an infected person sneezes or coughs, the flu virus is released into the air and can infect another person by way of their eyes, nose or mouth. When an object such as a doorknob, phone or railing is contaminated with droplets of the virus, infection can also occur by touching these objects.
Does the Flu Spread Between Species?
Because it circulates among so many different types of animals, influenza A has the potential to spread from one species to another. This transfer may happen through contact between different species and sometimes involves a process called reassortment. Reassortment occurs when different viruses mix their genes. For example, if a pig was infected with both a bird flu and a human flu strain, those two viruses could mix and create a new virus. This type of abrupt, major change in the influenza A virus is called antigenic shift. In rare cases, antigenic shifts can cause influenza pandemics, as the new virus would contain surface proteins (hemagglutinin and/or neuraminidase) previously unseen in human viruses. As a result, humans would not be immune, creating the potential for an influenza pandemic. However, transmission of influenza A from animals to humans — through contact or reassortment — is rare.
Treatment
For many people, influenza can be treated by staying at home, resting and drinking fluids. For those in higher-risk groups, such as the elderly and young children, doctors may also prescribe antiviral drugs. These drugs work to make symptoms milder, shorten the length of the illness and help prevent complications such as pneumonia.
Prevention and the Flu Vaccine
The flu can be prevented through frequent and thorough hand-washing, staying away from others during illness, and a healthy lifestyle (sufficient sleep, nutritious diet, plenty of liquids, stress management and moderate exercise).
The flu can also be prevented by receiving a flu vaccine. Each year, a new flu vaccine is created based on what researchers think will be the most common strains circulating in the upcoming flu season. Only influenza A and B strains are included in flu vaccines, as influenza C causes milder, more localized outbreaks. For example, in 2015–16, the World Health Organization recommended a flu vaccine containing four strains: A/California/7/2009 (H1N1), A/Switzerland/9715293/2013 (H3N2), B/Phuket/3073/2013 and B/Brisbane/60/2008. By comparison, the four-strain vaccine for 2016–17 was the same as the previous year, with the exception of the Switzerland strain, which was replaced by A/Hong Kong/4801/2014 (H3N2).
The effectiveness of the flu shot depends in part on how closely the influenza strains in the vaccine correspond with the strains circulating in any given year. In years where the viruses in the vaccine match the viruses that are circulating, effectiveness is between 50 and 60 per cent (meaning that the vaccine reduced the risk of influenza by 50 to 60 per cent among the overall population). In years where there is a mismatch, effectiveness can be much lower. In 2013–14, for example, the most common viruses were A/Texas/50/2012 (H3N2)-like viruses. Based on its prevalence, scientists recommended this same virus be included in the following year’s vaccine. However, different strains of the H3N2 virus were predominant during the 2014–15 flu season, meaning the vaccine’s effectiveness for that year was low. Viruses mutate quickly, making it difficult to predict which strains will be prevalent in the upcoming season.
Influenza Epidemics and Pandemics
A pandemic occurs when a disease spreads around the world, while an epidemic refers to widespread disease within a specific area or community. In Canada, influenza appeared in epidemic proportions on several occasions prior to the 20th century, particularly among Indigenous communities who had no immunity to the disease. Influenza epidemics often occurred during outbreaks of other diseases, including the 1847 typhus epidemic in Montréal and a 1900 epidemic of measles and influenza that began in Alaska and spread into the Yukon. In terms of influenza pandemics, experts believe that there have been about 14 since 1500, some of which spread to North America. Since Confederation, five pandemics have affected Canada: the 1890 Russian flu, the 1918 Spanish flu, the 1957 Asian flu, the 1968 Hong Kong flu and the 2009 H1N1 pandemic.
1890: Russian or Asiatic Flu in Canada
The Russian or Asiatic flu (likely caused by an H3Nx virus) began in the Eurasian Steppes, spread across Russia and Europe and arrived in northeastern North America in December 1889. By 1890, it had reached Canada, including the cities of Montréal, Toronto, Hamilton, Ottawa, London, Winnipeg and Vancouver. Although less lethal than the 1918 Spanish flu, some experts believe that exposure to the 1890 flu made patients more susceptible to severe outcomes (including death) during the 1918 pandemic.The theory centres on the concept of “original antigenic sin,” which suggests that for rapidly changing viruses such as influenza, the body may rely on antibodies developed in response to an earlier strain, thus compromising its response to the new virus.
1918: Spanish Flu in Canada

The most damaging epidemic of influenza — for Canada and the world — appeared during the First World War. The Spanish flu of 1918–19 killed between 20 and 100 million people, including about 30,000–50,000 Canadians. Unlike most strains of influenza, which are dangerous for those with reduced immunity (e.g., the elderly, the very young and those with pre-existing conditions), the 1918 Spanish flu tended to kill the young and hearty. Pneumonia contracted by a patient weakened by influenza rather than influenza itself was the major cause of death. A long-term consequence for some victims was the development of a parkinsonian syndrome, including a marked tremor.
The Spanish flu was brought into Canada by returning troops and made its way into even the remotest communities. Some entire villages were wiped out by the disease, and Labrador and Québec were particularly hard hit. Some areas unsuccessfully tried quarantine. All medical facilities and personnel were soon overtaxed and volunteers organized infirmaries in schools and hotels.
The epidemic brought not only death but social and economic disruption as well. Children were left parentless and many families found themselves without their chief wage earner. Armies on both sides of the war were temporarily debilitated. Businesses lost profits because of lack of demand for their products or because they were unable — as a result of a reduced work force — to meet the demand. Municipal governments, in an attempt to halt the spread of the disease, closed all except necessary services, and provinces enacted laws regarding quarantine and enforced the wearing of masks in public. Although the Canadian population unhappily accepted these restrictions, it defied the federal government’s request that First World War victory celebrations be postponed until 1 December. The establishment of the federal Department of Health in 1919 was a direct result of the epidemic.
The Spanish influenza strain, although decreasingly virulent, remained active in Canada until the mid-1920s. It has since been identified as an H1N1 virus.
1957: Asian Flu in Canada
In 1957, an outbreak of an H2N2 virus occurred in southern China, and spread swiftly around the world. The virus featured both a hemagglutinin and a neuraminidase protein previously unseen in humans. The 1957 outbreak also marked the first time a vaccine was prepared for a pandemic. The Asian flu led to an estimated 1–2 million deaths worldwide, some 7,000 of which occurred in Canada.
1968: Hong Kong Flu in Canada
The Hong Kong influenza pandemic began in 1968 in Southeast Asia. It was dubbed the “Hong Kong flu” as the outbreak there was the first to garner the attention of Western media. Caused by an H3N2 subtype, the virus had the same neuraminidase protein as the 1957 pandemic virus, but a different hemagglutinin protein. As a result, the virus’s impact varied depending on the region, as certain people were immune to at least part of the virus.The Hong Kong flu caused some 1–4 million deaths worldwide, and an estimated 4,000 in Canada.
2009: H1N1 in Canada
The H1N1 flu virus was first reported in Mexico in February 2009. Initially referred to as the “swine flu,” the virus had never been seen before in either animals or humans, but was thought to be most closely related to influenza viruses found in pigs in North America and Eurasia. Later, scientists discovered that in addition to elements of North American and Eurasian swine flu, the virus also contained aspects of North American bird and human influenza.
On 26 April 2009, Canada’s Public Health Agency reported its first case of H1N1. By 11 June 2009, 74 countries had laboratory-confirmed cases of the virus, and the World Health Organization announced a pandemic. Unlike the seasonal flu common during the winter, many Canadians contracted H1N1 during the summer months. A second wave of the virus followed in the winter of 2009; however, by January 2010 the Public Health Agency had begun to de-escalate its response to the pandemic.By July 2010, more than 200 countries or territories reported cases of the virus. More than 18,000 people were confirmed to have died of H1N1 worldwide, 428 of whom were Canadian. However, estimates based on statistical models have put the actual number of deaths worldwide in the hundreds of thousands.

 Share on Facebook
Share on Facebook Share on X
Share on X Share by Email
Share by Email Share on Google Classroom
Share on Google Classroom