Portrait of Dr. Frances Oldham Kelsey (date unknown)
Education
Frances Oldham was born in Cobble Hill on Vancouver Island, the daughter of a retired British army officer. She received a Bachelor of Science (1934) and a Master of Science (1935) from McGill University. Following graduation, she continued working with her supervisor, pharmacology professor Dr. Stehle.
In 1936, Stehle encouraged her to apply for a research assistantship or PhD position with Dr. E.M.K. Geiling at the University of Chicago. Geiling, who was setting up a new pharmacology department, wrote back to “Mr. Oldham,” offering a research assistantship and scholarship in the PhD program. His mistake troubled her: years later, she remarked that
[t]here was just one thing that bothered me a little about that letter. It started out, "Dear Mr. Oldham," and here my conscience tweaked me a bit. I knew that men were the preferred commodity in those days. Should I write and explain that Frances with an "e" is female and with an "i" is male? Dr. Stehle said, "Don't be ridiculous. Accept the job, sign your name, put Miss in brackets afterwards, and go!" That is what I did, and, to this day, I do not know if my name had been Elizabeth or Mary Jane, whether I would have gotten that first big step up. My professor at Chicago to his dying day would never admit one way or the other.
Oldham began her studies at the University of Chicago in March 1936. While working with Geiling, she was involved in the study of Sulfanilamide, a drug that had been very successful in treating pneumonia and streptococcus and staphylococcus infections. In order to make the drug easier to take and more palatable for children, one manufacturer decided to make a liquid solution. As sulfanilamide is not soluble in water or alcohol, the company used diethylene glycol (antifreeze); the solution was put on the market without testing. Fatalities were soon reported and the FDA seized as much of the product as they could find.
As the FDA did not have the necessary scientific expertise or facilities at the time, they requested Geiling’s help in determining whether sulfanilamide or the solvent was to blame for the deaths. As Geiling’s student, Oldham was tasked with monitoring animal studies, which quickly showed that diethylene glycol was to blame. The case led to passage of the 1938 Food, Drug, and Cosmetic Act.
The same year, Oldham received her PhD in pharmacology from the University of Chicago.
Early Career
Frances Oldham continued postgraduate work with the pharmacology department at the University of Chicago. During the Second World War, she was part of a research team tasked with finding and testing new antimalarial drugs. She also met Dr. Fremont Ellis Kelsey, a fellow faculty member, whom she married in 1943. However, the university had a policy that no department could employ two members of the same family. Frances Oldham Kelsey therefore decided to begin medical studies in 1946. She gave birth to two daughters while in medical school and received her MD in 1950.
Kelsey had little interest in practising medicine, and upon graduation became an editorial associate at the Journal of the American Medical Association. In 1952, her husband was offered a position as head of the pharmacology department at the University of South Dakota Medical School in Vermillion. Like the University of Chicago, South Dakota policy was that no two family members could teach in the same department. Kelsey therefore began a medical internship at a nearby hospital, followed by a three-year teaching fellowship paid for by a large drug firm. This external funding allowed her to be involved in teaching and research at the university from 1954 to 1957. After her fellowship ran out, she continued research on a voluntary basis, and on occasion filled in for medical doctors who were on vacation or at conference.
In 1960, Kelsey and her family moved to Washington, DC, to take up a position with the Food and Drug Administration; her husband secured a position with the National Institutes of Health.
Thalidomide
A month after she started working for the FDA, Frances Oldham Kelsey was assigned to the Bureau of Medicine as a reviewing officer for new drug applications. One of her first reviews was an application by the Merrell Company to sell thalidomide in the United States. Thalidomide, an immunomodulatory drug, was developed in Germany in the 1950s. It was originally prescribed as a sedative, but was soon given to pregnant women to alleviate nausea. By 1960, it was widely used in Europe and across the world (including Canada).
However, Kelsey and two of her colleagues at the FDA (a chemist and a pharmacologist) had questions about thalidomide’s safety and felt that studies had been both insufficient and inconclusive. Kelsey was also concerned by a report in the British Medical Journal of side effects in patients who regularly took the drug. She also suspected that thalidomide could harm fetuses. Kelsey therefore withheld approval of thalidomide, effectively blocking the sale of the drug, which had already been given to some American patients during clinical trials.
Kelsey’s concerns were validated in November 1961, when reports emerged from Germany and the United Kingdom that mothers who had taken thalidomide during pregnancy were having babies with severe birth defects. The most striking was the limb malformation known as phocomelia, in which the hands or feet (or both) start from the main joint (that is, the shoulder or the hip). Babies were also born with cleft palate, abnormal or missing ears, kidney problems, heart problems, digestive system disorders, and defects of the spinal cord. By the end of December 1961, the drug had been withdrawn from the markets in both West Germany and the United Kingdom.
Dr. Helen Taussig, an American pediatric cardiologist, travelled to Germany to investigate these reports and concluded that thalidomide was indeed to blame for the outbreak of congenital deformities there. In 1962, she wrote an article titled “A Study of the German Outbreak of Phocomelia” in the Journal of the American Medical Association. This article, and her testimony before Congress, was instrumental in helping Kelsey to permanently ban the sale of thalidomide in the United States. (In 1998, the FDA approved thalidomide for the treatment of erythema nodosum leprosum, a complication of leprosy.)

Dr. Frances Oldham Kelsey, pictured with a set of scales.
Career in the FDA
Frances Oldham Kelsey’s involvement in the thalidomide case contributed to improved drug regulations in the United States. In 1962, the government enacted the Kefauver-Harris Drug Amendments, which required that 1) drugs had to be shown to be both safe and effective; 2) adverse reactions had to be reported to the FDA; and 3) informed consent had to be obtained from patients involved in clinical trials.
Kelsey continued her work with the FDA until 2005, when she was over 90 years old. Throughout her decades of service, she worked tirelessly to protect American patients. In 1967, the FDA created the Division of Scientific Investigations, which was responsible for inspecting clinical investigators, animal studies, and institutional review boards involved in drug trials. Kelsey was the division’s first director and remained in that post until 1995. That year, at 81 years of age, she became deputy for scientific and medical affairs in the Office of Compliance (part of the FDA’s Center for Drug Evaluation and Research).
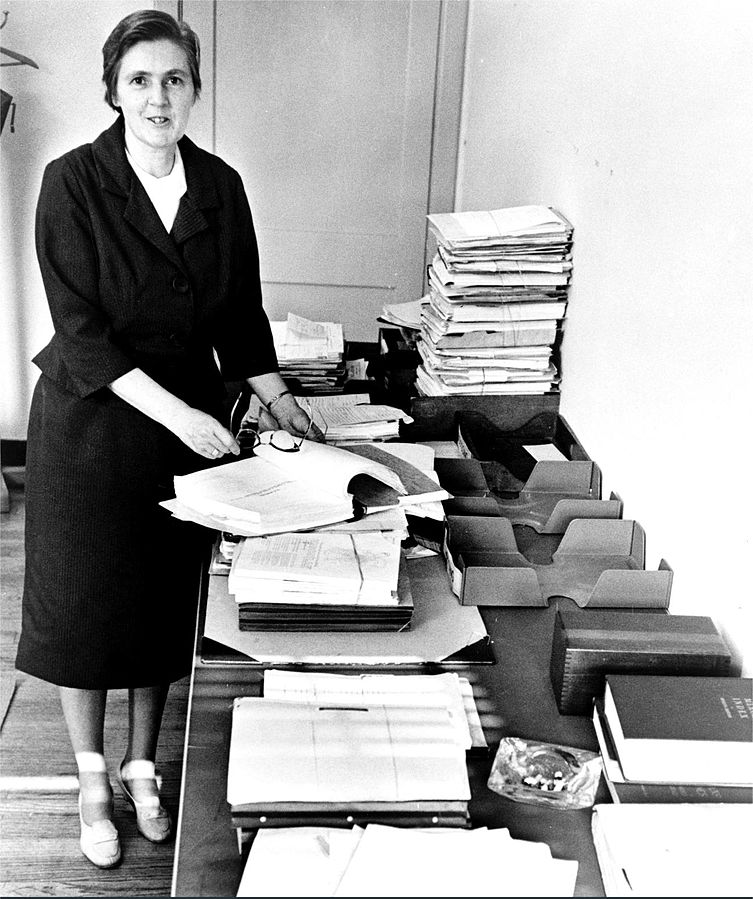
Dr. Frances Oldham Kelsey, pictured here in the 1960s, spent most of her career at FDA overseeing scientific investigations of drugs.
Honours
On 7 August 1962, Frances Oldham Kelsey received the President’s Award for Distinguished Federal Civilian Service from President John F. Kennedy. During the presentation, she was commended for
her exceptional judgment in evaluating a new drug for safety for human use [that] prevented a major tragedy of birth deformities in the United States. Through high ability and steadfast confidence in her professional decision, she made an outstanding contribution to the protection of the health of the American people.
Kelsey received many other honours in the United States: in 2000, she was inducted into the National Women’s Hall of Fame, and in 2001, she became a virtual mentor for the American Medical Association. In 2006, she was given the Foremother Award by the National Research Center for Women and Families. In 2010, 50 years after Kelsey received the thalidomide application, the FDA created an annual award in her honour. She is less well-known in Canada, although the town of Mill Bay, British Columbia, named a secondary school after her in the 1990s. On 6 August 2015, Kelsey was invested into the Order of Canada; she died the following day. Asteroid (6260) Kelsey was named in her honour.

Dr. Frances Kathleen Oldham Kelsey receiving the President's Award for Distinguished Federal Civilian Service from President John F. Kennedy, in 1962.
Legacy
Frances Oldham Kelsey’s professionalism, insight and strength of character likely saved thousands of American children from severe deformities and disabilities. It is estimated that over 10,000 children in 46 countries were born with deformities because of thalidomide (it is unknown how many babies died, were stillborn, or miscarried because of the drug).
Thalidomide in Canada
In Canada, over 100 children were born with severe defects caused by thalidomide. The drug became available as a sample in late 1959, and as a prescription medication in April 1961 after it was approved for sale by the Department of Health and Welfare. It continued to be sold on the Canadian market until March 1962, three months after it was pulled from the shelves in West Germany and the United Kingdom. According to the Thalidomide Victims Association of Canada (TVAC), it was still available in some pharmacies until the middle of May 1962.
In the 1990s, 109 Canadian thalidomide victims received lump-sum payments of between $52,000 and $82,000 from the federal government. However, these funds have proven insufficient to cover the medical needs of survivors. Therefore, in 2014, the TVAC requested additional government compensation: a $250,000 lump-sum payment followed by annual payments of between $75,000 and $150,000. In March 2015, the federal government announced a $125,000 lump-sum settlement each for eligible thalidomide survivors under the Thalidomide Survivors Contribution Program (TSCP). Two months later, in May 2015, survivors learned that they would receive an annual pension from the government of up to $100,000 a year, depending on their disability. Eligible thalidomide survivors could also access an Extraordinary Medical Assistance Fund (EMAF), which would help pay for medical expenses that are not covered by provincial and territorial health plans, such as specialized surgery, or adjustments to homes and vehicles.
However, thalidomide survivors argued that this funding was inadequate. In December 2017, a new organization, the Thalidomide Survivors’ Task Group, demanded that the federal government double the compensation that it provided under the TSCP. In January 2019, federal minister of health Ginette Petitpas Taylor announced that the government would launch a new program in the spring of 2019. The Canadian Thalidomide Survivors Support Program (CTSSP) will replace the existing program (TSCP) and provide a tax-free lump-sum payment of $250,000, as well as ongoing tax-free payments, to eligible survivors. The government also recognized that some survivors may have been excluded due to the TSCP’s eligibility criteria and indicated that the new CTSSP would “provide a fair and comprehensive approach to identifying thalidomide survivors that is based on international best practices.” Finally, more funds would be available through the EMAF, which was increased from $500,000 to $1,000,000 per year.

 Share on Facebook
Share on Facebook Share on X
Share on X Share by Email
Share by Email Share on Google Classroom
Share on Google Classroom