Assisted suicide is the intentional termination of one’s life, assisted by someone who provides the means or knowledge, or both. (See also Suicide.) Between 1892 and 2016, assisted suicide was illegal in Canada under section 241(b) of the Criminal Code. In 2015, after decades of various legal challenges, the Supreme Court of Canada decided unanimously to allow physician-assisted suicide. In June 2016, the federal government passed the Medical Assistance in Dying (MAID) Act, which established the eligibility criteria and procedural safeguards for medically assisted suicide. In March 2021, new legislation was passed that expanded eligibility for MAID.
This article contains sensitive material that may not be suitable for all audiences.
Background and Criminal Code
When the Criminal Code was introduced in Canada in 1892, suicide and attempted suicide were considered criminal offences under section 241(b). While suicide was decriminalized in 1972, assisted suicide remained illegal. Anyone found guilty of counselling someone to take their own life or aiding someone to take their own life was guilty of culpable homicide and liable to imprisonment of up to 14 years. Much debate followed in provincial and federal legislatures concerning the right of individuals to physician- or other-assisted suicide, particularly in cases where the person is too disabled to perform the act without assistance.
The Difference Between Assisted Suicide and Euthanasia
Although assisted suicide is sometimes called voluntary, or active, euthanasia, the two are, in fact, different. Assisted suicide is when someone provides the knowledge or means to help someone end their own life. For example, assisted suicide would include a physician providing drugs to a patient, who then uses those drugs to kill herself. Euthanasia, however, involves someone deliberately acting to cause the death of someone else to end their suffering; the act itself is the direct cause of death. Euthanasia can be voluntary, involuntary (the person did not provide consent) or non-voluntary (the person could not provide consent). An example of euthanasia would be a doctor administering the drugs that end someone’s suffering and result in their death.
Sue Rodriguez Challenges Assisted Suicide Law (1993)
In the early 1990s, Sue Rodriguez submitted to the courts that section 241(b) of the Criminal Code, which prohibited assisted suicide, was constitutionally invalid. Rodriguez suffered from amyotrophic lateral sclerosis (ALS) and wanted the legal right to have a physician’s help in ending her own life at a time of her choosing. After losing her challenge in both the Supreme Court of British Columbia and the British Columbia Court of Appeal, Rodriguez took her case to the Supreme Court of Canada.
On 30 September 1993, a 5–4 majority of Supreme Court justices upheld the status quo, affirming that the provision was constitutional and did not violate the Canadian Charter of Rights and Freedoms. The decision conformed to the principle of fundamental justice based on the idea that assisted suicide is intrinsically blameworthy on moral and legal planes and could lead to abuses. However, the four minority judges argued that the prohibition of assisted suicide was arbitrary. In effect, a physically able person can die by suicide (which is not a criminal act), while a physically disabled person commits a crime when she asks for assistance to perform the same act. In their opinion, this distinction was contrary to the principles of fundamental justice.
Rodriguez died by suicide in February 1994, assisted by an anonymous doctor in the presence of NDP MP Svend Robinson, who had championed her cause. (See also Assisted Suicide in Canada: The Rodriguez Case.)
Euthanasia and the Robert Latimer Case (1994)
In November 1993, Robert Latimer was charged with the murder of his severely disabled daughter, Tracy. Tracy’s oxygen supply was cut off during birth, causing severe brain damage and recurring seizures. After years of medication and painful operations, her parents were informed in October 1993 that their 12-year-old daughter would require further surgeries. The thought of his daughter’s continued distress led Latimer to end Tracy’s life. On 24 October 1993, he placed Tracy in his truck, asphyxiating her with exhaust fumes.
When the autopsy showed that Tracy had died from carbon monoxide poisoning, Latimer confessed that he had ended her life but insisted that he had not murdered her. However, on 16 November 1994, he was convicted of second-degree murder and sentenced to life imprisonment with no parole for 10 years (a decision upheld by the Saskatchewan Court of Appeal). He was retried in February 1997, by order of the Supreme Court of Canada, and was again found guilty of second-degree murder. (See also Robert Latimer Case.)
Latimer’s case was first argued in the courts in November 1994, about a year after Sue Rodriguez lost her case in the Supreme Court. Many sympathized with Latimer, as they did with Rodriguez. However, the cases were different in an important way: Latimer’s action could best be described as non-voluntary euthanasia (the deliberate act of ending someone else’s life without their consent), while Rodriguez wanted a physician’s assistance in ending her own life.

Physician-Assisted Suicide Becomes Legal in Canada (2015)
In 2011, the British Columbia Civil Liberties Association (BCCLA) filed a lawsuit that challenged the law against assisted suicide, arguing that the prohibition violated sections 7 and 15(1) of the Canadian Charter of Rights and Freedoms (guaranteeing, respectively, the right to “life, liberty and security of person” and equality). The case was brought to court on behalf of the families of Kay Carter, who suffered from degenerative spinal stenosis, and Gloria Taylor, who had ALS (Carter died in 2010; Taylor, in 2012). In June 2012, the Supreme Court of British Columbia ruled in favour of the plaintiffs. However, the federal government appealed the ruling and, in October 2013, the Court of Appeal for British Columbia overturned it. The BCCLA then appealed to the Supreme Court of Canada.
When Carter v. Canada came before the Supreme Court in 2014, the national and international context had changed significantly since the Rodriguez v. British Columbia decision (1993). In 1993, assisted suicide was illegal in all countries except Switzerland, where it was legal unless motivated by selfish reasons; in the Netherlands, assisted suicide was officially illegal, but physicians were not prosecuted as long as they followed strict guidelines. By 2014, however, the situation had changed: the Netherlands, Belgium, Luxembourg and the states of Oregon, Washington and Vermont had passed legislation that allowed assisted suicide in certain circumstances.
Meanwhile, in June 2014, the province of Quebec passed legislation that legalized “medical aid in dying” for “consenting adult patients who suffer from an incurable illness, an advanced state of irreversible decline in capability, and constant and unbearable suffering.” By 2015, therefore, legal precedents had been set both in Quebec and internationally, and there was greater public support for decriminalizing assisted suicide.
On 6 February 2015, the Supreme Court voted unanimously (9–0) to allow physician-assisted suicide for “a competent adult person who (1) clearly consents to the termination of life; and (2) has a grievous and irremediable medical condition (including illness, disease or disability) that causes enduring suffering that is intolerable to the individual in the circumstances of his or her condition.” The court reasoned that the Criminal Code prohibition was unconstitutional because it breached the rights to life, liberty and security of the person, as enshrined in section 7 of the Charter. The Supreme Court gave Parliament 12 months to draft a new law concerning assisted suicide. However, no such law had been drafted by the time the Conservative government of Stephen Harper left office in October 2015.
Medical Assistance in Dying (MAID) Act, 2016
In January 2016, the Supreme Court granted a four-month extension to the new Liberal government under Justin Trudeau. At the same time, it established a constitutional exemption that allowed individuals to apply for judicial authorization to access physician-assisted dying, provided that they met the criteria set out in the 2015 Supreme Court decision. On 6 June 2016, with no new law in place, physician-assisted suicide became legal in Canada. At the time, the House of Commons had passed Bill C-14, but the proposed legislation was still being debated in the Senate.
On 17 June 2016, more than a year after the Supreme Court decision, Bill C-14 became law. The Medical Assistance in Dying (MAID) Act established the procedural safeguards and eligibility criteria for medically assisted suicide: those eligible have to be at least 18 years of age, with a “grievous and irremediable medical condition” that causes “enduring physical or psychological suffering that is intolerable” to them. Moreover, they must be in an “advanced state of irreversible decline,” in which their “natural death has become reasonably foreseeable.”
The law included a number of safeguards. First, the medical or nurse practitioner had to confirm that the person met all eligibility criteria for Medical Assistance in Dying (MAID). A second assessment had to be done by an independent practitioner. The request had to be made in writing after the patient was informed that their natural death was reasonably foreseeable. The request had to be signed and dated in the presence of two independent witnesses. Patients had to be informed that they could withdraw their request at any time. There had to be a period of at least 10 days between the written request and the provision of MAID. Finally, the practitioner had to confirm the person’s consent immediately before providing assistance.
Critics pointed out that the legislation was more restrictive than the Supreme Court decision and that it might be vulnerable to constitutional appeal.
Challenges and Amendments
In January 2019, two Montrealers, Jean Truchon and Nicole Gladu, launched a court challenge seeking access to medically assisted death under Quebec and federal legislation. Both individuals had degenerative diseases that they said caused “persistent and intolerable suffering.” They argued that the existing legislation was too narrow and deprived them of their Charter rights.
In September 2019, a Superior Court of Quebec justice agreed with the plaintiffs and ruled that the precondition for assisted death — that natural death was “reasonably foreseeable” — was unconstitutional. Justice Christine Baudouin ruled that the provision “infringes life, liberty and security of the person guaranteed by Section 7 of the Charter…and deprives [individuals] of their autonomy and their choice to end their lives at the time and in the manner desired.” The court gave both the Quebec and federal governments six months to respond to its decision. (In March 2020, the Quebec government simply dropped the problematic provision.)
The Quebec court’s decision was praised by some but opposed by others, including groups representing people with disabilities. Both Living with Dignity (Vivre dans la dignité) and the Collective of Doctors Against Euthanasia (Collectif des Médecins contre l’euthanasie) intervened in the case.
In February 2020, the Liberal government introduced Bill C-7, which proposed to allow Medical Assistance in Dying (MAID) for those whose natural death was “not reasonably foreseeable.” It would, however, continue to prohibit MAID for individuals whose only underlying condition was mental illness. The bill established safeguards for the two different tracks — that is, for those whose natural death was reasonably foreseeable and for those whose death was not reasonably foreseeable.
However, discussion of Bill C-7 was stalled by the COVID-19 pandemic, which disrupted parliamentary proceedings. The House of Commons adjourned in mid-March 2020 because of the pandemic. In June 2020, the federal government requested an extension to comply with the court order to expand access to MAID. The new deadline was set for 18 December 2020. The bill died when Prime Minister ^House of Commons by a vote of 212 to 107 on 10 December 2020. It was then debated in the Senate, which approved the bill with amendments in February 2021. The federal government modified some of the amendments and presented a revised version of Bill C-7 in March. It was passed by the House of Commons and the Senate and became law on 17 March 2021.
MAID, 2021
On 17 March 2021, the revised MAID legislation came into effect. The new law removed the requirement that a person’s natural death must be reasonably foreseeable in order to be eligible for MAID. It also introduced a two-track approach to procedural safeguards, depending on whether or not a person’s natural death was reasonably foreseeable.
The original safeguards would apply for patients whose natural death was reasonably foreseeable, with two exceptions. First, the patient’s written request only has to be signed by one independent witness (not two, as under the original law). Second, the requirement for a 10-day reflection period was removed. The new law also changed to the requirement for “final consent,” waiving that requirement for those whose natural death was reasonably foreseeable and who provide consent in advance but who may lose the capacity to consent. These changes were intended to prevent people from ending their lives sooner than they might want due to fears of losing their ability to give consent.
The safeguards also apply to patients whose natural deaths are not reasonably foreseeable. Such persons are also subject to four new or clarified safeguards. First, the new legislation requires a minimum 90 days’ assessment period for a person’s eligibility for MAID. This period can be shortened if the individual will soon lose the capacity to make health care decisions. Second, at least one of the two mandatory assessments must be performed by a doctor or nurse practitioner who has expertise in the medical condition causing the patient’s suffering or consults with a practitioner who has such expertise. Third, the patient must be informed of available counselling and support services and offered consultation and access to such services. Fourth, the patient and practitioners must agree that they had discussed and seriously considered ways to alleviate the patient’s suffering before MAID could be provided.
The 2021 MAID legislation also includes a new provision for those who choose to self-administer a substance for medically assisted death. Under the revised legislation, such persons can arrange for practitioner-assisted MAID in the event of complications — that is, individuals can provide consent to their practitioner for MAID if their self-administered attempt results in the loss of decision-making capacity but not in death.
MAID and Mental Illness
The 2021 MAID legislation temporarily excludes persons suffering only from mental illness. This includes conditions such as depression and personality disorders but not neurocognitive and neurodevelopmental disorders. The exclusion will end on 17 March 2023. In the intervening time, the government must initiate a review by experts, who will make recommendations within a year (by 17 March 2022) on the protocols, guidance and safeguards for individuals suffering from mental illness.
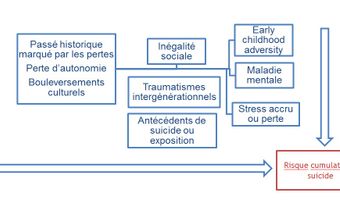
See also Suicide in Canada; Fighting Depression-related Suicide; Suicide Among Indigenous Peoples in Canada.

 Share on Facebook
Share on Facebook Share on X
Share on X Share by Email
Share by Email Share on Google Classroom
Share on Google Classroom