An epidemic occurs when an infectious disease spreads rapidly throughout a community at a particular time. Several epidemics have occurred over the course of Canadian history, the most disastrous being those which affected Indigenous peoples following the arrival of Europeans.
Click here for definitions of key terms used in this article.

Background
The application of the principles of hygiene in recent decades has virtually eliminated epidemic outbreaks of the most deadly contagious diseases. Historically, however, epidemic diseases in North America were initially spread from European explorers to Indigenous peoples. Later, the unhealthy conditions of ships which linked the Americas to Europe favoured the development of contagious diseases such as smallpox, typhus, cholera and influenza among their passengers. Ignorance of the causes of these diseases and how they were transmitted helped spread them into port cities. The outbreak of an epidemic almost always coincided with the arrival of a vessel full of sick passengers.
European Contact with Indigenous Peoples
When Europeans began arriving on the shores of the Americas, the epidemic diseases they brought with them set off one of the largest depopulations in human history. Prior to European arrival, diseases such as smallpox, measles and yellow fever did not exist in these regions of the world. Having never been exposed to these illnesses, Indigenous peoples did not have the antibodies needed to ward off infection. Using Christopher Columbus’ arrival in the Americas in 1492 as a starting point, Indigenous populations were drastically reduced by epidemic disease over the course of the next 400 years, as Europeans continued to explore new territory and came into contact with different communities.
Of all the diseases that affected Indigenous peoples, smallpox was often the worst. While every encounter with European disease cannot be catalogued here, two stories serve as notable examples. When travelling the St Lawrence River, Jacques Cartier observed well-established, heavily populated communities at Stadacona, an Iroquoian village located at what is now Québec City. Not long after his arrival, in the winter of 1535, he noted that Iroquoians were dying of an illness he and his own men seemed immune to. Later historians would identify the illness as smallpox. About 70 years later, when Samuel de Champlain explored the same route in 1603, Stadacona was a ghost town.
Another incident speaks to the intentional spread of disease. In 1763, as Odawa chief Obwandiyag (Pontiac) began his resistance movement against British rule, Sir Jeffery Amherst, leader of the British army, suggested to Col. Henry Bouquet that smallpox be introduced via infected blankets given to the First Nations they were fighting. He wrote, “You will do well to try to inoculate the Indians by means of blankets as well as to try every other method that can serve to extirpate this exorable race.” Several historians note there is no evidence that Bouquet or any of his men carried out the act. That same year, however, William Trent, a trader at Fort Pitt (located in present-day Pittsburgh, Pennsylvania) wrote of a meeting with two members of the Delaware Nation, “we gave them two Blankets and a Handkerchief out of the Small Pox Hospital. I hope it will have the desired effect.”
Estimations of the number of Indigenous peoples in the Western hemisphere at the time of Columbus’ arrival vary widely, and for this reason it is difficult to say exactly how many died of the diseases Europeans introduced. However, some scholars estimate that, by around 1900, Indigenous populations had declined by upwards of 93 per cent. Though other factors contributed to their depopulation (e.g., war, dispossession), epidemic disease was easily the most devastating.
Smallpox
By the end of the 18th century inoculation against smallpox had become a popular preventive method in Europe. Smallpox inoculation meant smallpox pus was introduced beneath a patient’s skin. Soon after, vaccination (more effective and less dangerous) appeared in North America. Yet, epidemics of smallpox continued to affect the population. Montreal was hit particularly hard (see The 1885 Montreal Smallpox Epidemic). The epidemic of 1885 was especially dramatic; its scale persuaded municipal authorities to make vaccination obligatory, but medical opinion divided into pro- and anti-vaccination camps, with the latter accusing the former of spreading the disease. The population, terrified, refused to be vaccinated. (See also Vaccination and Vaccine Hesitancy in Canada.) On 18 September 1885 a riot broke out in the city. People tore down pro-vaccination posters and ransacked the home of the official medical vaccinator, city hall, pharmacies and the homes of municipal magistrates. The extent of the catastrophe (it took 3,164 lives, 2,117 of them children) eventually prompted Montrealers to obey the sanitary authorities and the clergy.
Typhus
Typhus first reached Canada in 1659, but the outbreak of 1746 was notable for its severity. France had sent a large flotilla of warships to Canada to retake Port-Royal in Acadia. Of the 3,150 soldiers aboard, 1,270 died at sea and another 1,130 in Bedford Basin, where they were supposed to rendezvous with an army coming from Quebec. The disease hit the Mi'kmaq of the region and more than one-third died.
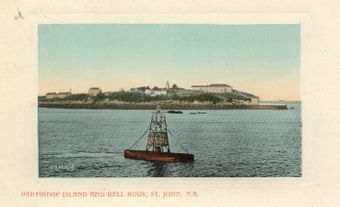
In 1847, 9,293 immigrants from the British Isles (particularly those of Irish descent) died during the Atlantic crossing, causing the year to be dubbed "the year of the typhus." (See also Immigration to Canada.) Another 10,037 died at Grosse- Île, the quarantine station in the St Lawrence River below Quebec, or in the hospitals of Québec, Montreal, Kingston and Toronto. Monuments at Cap des Rosiers on the Gaspé coast commemorate those who died at sea. (See also Irish Canadians.)
Cholera
The Canadian government feared the introduction of cholera by European immigrants, especially in 1831, when cholera was devastating Europe. New regulations forbade the local population to visit ships in port. A sanitation committee was set up early in 1832, quarantine laws were strengthened and Grosse Île was placed under military command. However, one ship was permitted to leave the quarantine station and was responsible for the cholera epidemic in 1832, when some 6,000 people died. Barely two years later the disease struck again, and sporadic outbreaks occurred throughout the century.
Influenza
While throughout the history of Canada influenza mortality has generally been low, some epidemics occurred during outbreaks of typhus or other diseases. Since the 1918 influenza pandemic, scientific discoveries have rendered infectious diseases less deadly (see 1918 Spanish Flu in Canada). Recent influenza epidemics, for example, have caused much sickness but few deaths. Health Canada reports that immunizing high-risk persons, such as the elderly and very young, before each influenza season is the most effective measure for reducing influenza-related complications.

Yellow Fever
In 1710, a disease known today as yellow fever, arrived in the port of Québec from the West Indies. The vector insect is Stegomya fasciata. This mosquito found the heat and humidity on board ship ideal for its reproduction and infected the vulnerable passengers with the dangerous virus. The sick sailors were taken to Hôtel-Dieu in Québec, where they died — as did six nurses and 12 priests. The epidemic must have claimed many victims, but the exact number is unknown. Once winter came, the insect and its disease both disappeared. There do not seem to have been any other such epidemics in Canada, even if a few sporadic cases occurred in the country's port cities. The Canadian government has on occasion declared quarantine against American ports where the disease has raged.
Baie Saint-Paul Disease
In 1773, a mysterious disease appeared in the Baie Saint-Paul area that spread through neighbouring parishes and finally reached the Montreal region. Its symptoms included buccal (cheek lining) ulcers, pain in the limbs and finally the destruction of the bones of the nose, the palate, the gums and the appearance of swellings on the head, the clavicles and the bones of the limbs. Men, women and children were all afflicted. After some hesitation and discussion, medical opinion decided that this malady, known as the Baie Saint-Paul disease, was a form of syphilis (see Sexually Transmitted Infections).
Severe Acute Respiratory Syndrome (SARS)
Canada experienced an outbreak of severe acute respiratory syndrome (SARS) in 2003. SARS is an infectious disease caused by a coronavirus (SARS-CoV). It was unknown until a worldwide outbreak of the disease in 2002–03. Coronaviruses usually cause mild illnesses such as the common cold. The coronavirus that causes SARS, however, is more virulent. This means that it is better able to overcome the body’s defences.
The first case of SARS was reported in China in November 2002. The virus then spread to more than 20 countries, including Canada. Global travel helped to quickly spread the disease. According to the WHO, 8,096 people worldwide were infected during the outbreak (from 1 November 2002 to 31 July 2003). Of these, 774 died.
In Canada, the outbreak was largely centred in Toronto. It was mostly contained to hospitals, where health-care workers, the elderly and those with pre-existing illnesses ill were most at risk. During the outbreak, thousands of Canadians were quarantined. Many of these people voluntarily quarantined themselves in their homes. Airports in Toronto and Vancouver screened travellers for high fever. In total, there were 438 probable cases of SARS in Canada, resulting in 44 deaths. (See also SARS in Canada.)
In December 2019, a new type of novel coronavirus, SARS-CoV-2, was identified in Wuhan, China. The WHO announced “COVID-19” as the name of the disease on 11 February 2020. On 11 March 2020, The WHO declared COVID-19 a global pandemic with 118,000 cases of the virus being reported in 114 countries. A pandemic is an outbreak of an infectious disease that affects a large proportion of the population in multiple countries or worldwide. By 15 March, Canada reported 317 cases, including one death, from COVID-19. As of September 2022, the COVID-19 pandemic has caused more than 612 million confirmed cases and 6.5 million deaths globally, including over 4.2 million cases and 44,992 deaths in Canada. (See also Covid-19 Pandemic in Canada).
See also: Tuberculosis
Key Terms
Epidemic – A widespread outbreak of an infectious disease in a population at a particular time.
Pandemic – An outbreak of an infectious disease, usually caused by a new virus or bacterium, or a novel strain, that affects a large proportion of the population in multiple countries or worldwide.
Quarantine – The separation of an individual, or a group of people, from a surrounding population and the restriction of their movement to prevent the introduction and spread of a disease.
Virus – An organism, too small to be seen with a typical microscope, that can multiply inside the cells of its host and usually causes disease.

 Share on Facebook
Share on Facebook Share on X
Share on X Share by Email
Share by Email Share on Google Classroom
Share on Google Classroom